Table of Contents
Introduction
Wisdom tooth infections, clinically known as pericoronitis, are a common dental issue that typically affects individuals in their late teens to early twenties. These infections occur when the wisdom teeth, or third molars, begin to emerge through the gums, often resulting in partial eruption due to limited space in the mouth. This partial eruption creates an environment where bacteria can thrive, leading to inflammation and infection of the surrounding gum tissue.
The positioning of wisdom teeth plays a significant role in the onset of these infections. Unlike other teeth, wisdom teeth often emerge at awkward angles or become impacted, failing to fully break through the gum line. This misalignment can create pockets where food particles and bacteria accumulate, making it difficult to maintain proper oral hygiene. Consequently, the trapped debris and bacterial growth result in painful infections characterized by swelling, redness, and sometimes pus formation.
Wisdom tooth infections are particularly prevalent among young adults, a demographic in which the eruption of wisdom teeth commonly occurs. During this period, the jaws have usually stopped growing, limiting the space available for these additional molars. This lack of space can lead to overcrowding, impaction, and subsequent infection. Understanding the underlying causes and risk factors associated with wisdom tooth infections is crucial for timely intervention and management.
As we delve deeper into this topic, we will explore the various symptoms that indicate a wisdom tooth infection, the diagnostic methods employed by dental professionals, and the range of treatment options available. Additionally, preventive measures and best practices for maintaining oral health will be discussed to equip readers with comprehensive knowledge on managing and mitigating the risks associated with wisdom tooth infections.
Common Symptoms of Wisdom Tooth Infections
Wisdom tooth infections, often resulting from the partial eruption of these third molars, can manifest through various symptoms. Recognizing these symptoms early is crucial for timely intervention and management. One of the primary indicators of a wisdom tooth infection is localized pain. This pain can range from mild to severe and may radiate to the surrounding teeth and jaw.
Swelling and redness in the gums around the wisdom tooth are also common signs. The inflamed tissue can be tender to touch, and the swelling might extend to the cheek, causing noticeable discomfort. Another frequently observed symptom is bad breath, medically known as halitosis. This occurs due to the accumulation of bacteria and food particles in the inflamed area, leading to an unpleasant odor.
In more severe cases, individuals may experience difficulty opening their mouth, a condition known as trismus. This restriction in movement can significantly impact daily activities such as eating and speaking. Additionally, a fever may develop, indicating that the body is fighting off an infection. Swollen lymph nodes in the neck or under the jaw are another red flag, suggesting that the infection might be spreading beyond the immediate vicinity of the tooth.

It’s essential to monitor these symptoms closely, as they can escalate quickly. If you observe a combination of these signs, seeking prompt dental or medical attention is advised to prevent further complications. Early diagnosis and treatment can help manage the infection effectively, ensuring better oral health and overall well-being.
Potential Complications and Risks
Wisdom tooth infections, if left untreated, can lead to a host of complications that extend far beyond localized pain and discomfort. One primary risk involves the spread of the infection to adjacent teeth and tissues. This can result in abscess formation, where pus accumulates, causing significant swelling, pain, and potential damage to surrounding structures.
Moreover, the infection can extend to other parts of the mouth, including the gums and jawbone, leading to conditions such as cellulitis. Cellulitis is characterized by the inflammation of the soft tissues, resulting in redness, swelling, and tenderness, and can make basic activities like eating and speaking extremely painful.
An untreated wisdom tooth infection also poses the danger of spreading to the face and neck. Once the bacteria migrate to these areas, they can cause facial swelling and, in severe cases, Ludwig’s angina—a life-threatening condition marked by a rapid spread of infection under the tongue and jaw, obstructing the airway.
Perhaps most concerning is the risk of the infection entering the bloodstream, leading to sepsis. Sepsis is a severe and potentially fatal condition that triggers widespread inflammation throughout the body. Symptoms include fever, rapid heart rate, difficulty breathing, and confusion. Immediate medical intervention is crucial to manage this complication.
Given these risks, timely diagnosis and treatment of a wisdom tooth infection are paramount. Early intervention not only alleviates pain but also mitigates the progression of the infection, thereby preventing the onset of these severe complications. Regular dental check-ups and prompt attention to oral discomfort can significantly reduce the likelihood of encountering these risks and ensure overall oral health.
Medical Treatments for Wisdom Tooth Infections
Wisdom tooth infections, medically known as pericoronitis, often require professional intervention to manage effectively. Dentists and oral surgeons play a crucial role in diagnosing and treating these infections. The initial step generally involves a thorough examination and imaging studies such as X-rays to assess the extent of the infection.
One of the primary treatments for a wisdom tooth infection is drainage. This procedure involves making a small incision to drain the pus, alleviating pain and reducing swelling. Drainage is often accompanied by a course of antibiotics to combat the underlying bacterial infection. Antibiotics commonly prescribed include amoxicillin, clindamycin, or metronidazole, depending on the patient’s medical history and any potential allergies.
In cases where the infection is recurrent or severe, removal of the infected wisdom tooth may be necessary. This procedure, known as extraction, can be performed under local or general anesthesia. The complexity of the extraction depends on the tooth’s position and the extent of the infection. In some instances, an oral surgeon may need to perform a minor surgical procedure to remove the tooth, especially if it is impacted or has not fully erupted.
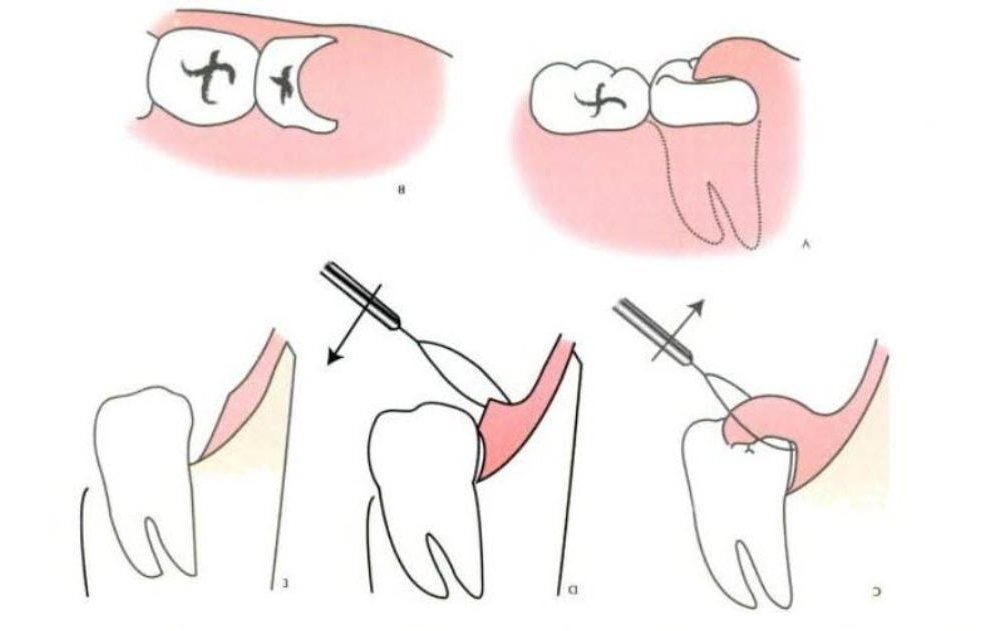
Other dental procedures may also be employed to manage wisdom tooth infections. For example, a dental cleaning can help remove debris and bacteria from around the infected area, reducing the risk of further infection. In some cases, a procedure called operculectomy may be performed. This involves removing the overlying gum tissue to prevent food particles and bacteria from getting trapped, thereby reducing the risk of infection.
Overall, the goal of medical treatments for wisdom tooth infections is to alleviate pain, eliminate the infection, and prevent future occurrences. It is essential for individuals experiencing symptoms of a wisdom tooth infection to seek prompt dental care to avoid complications and ensure effective treatment.
The Role of Antibiotics in Treating Infections
Antibiotics play a crucial role in managing wisdom tooth infections. These infections typically arise when the wisdom teeth, located at the back of the mouth, become impacted or fail to erupt properly. Consequently, bacteria can accumulate, leading to inflammation and infection.
Dentists often prescribe antibiotics to combat these bacterial infections. Commonly prescribed antibiotics include amoxicillin, clindamycin, and metronidazole.
- Amoxicillin, a broad-spectrum antibiotic, is frequently chosen for its efficacy against a wide range of bacteria.
- Clindamycin is another option, particularly for patients allergic to penicillin, as it targets anaerobic bacteria that thrive in low-oxygen environments.
- Metronidazole may be used in conjunction with other antibiotics to enhance their effectiveness against stubborn infections.
The effectiveness of these antibiotics largely depends on the specific bacteria causing the infection and the patient’s adherence to the prescribed regimen. Generally, antibiotics can alleviate symptoms and prevent the spread of infection. However, it is essential to complete the entire course, even if symptoms improve before the medication is finished. Prematurely stopping antibiotics can lead to the development of antibiotic-resistant bacteria, making future infections more challenging to treat.
While antibiotics are generally safe, they can cause side effects. Common side effects include gastrointestinal issues such as nausea, diarrhea, and stomach cramps. Some individuals may also experience allergic reactions, ranging from mild rashes to severe anaphylaxis. It is important to inform the prescribing dentist of any known allergies or previous adverse reactions to medications.
In summary, antibiotics are a vital component in treating wisdom tooth infections. Their proper use can significantly reduce the bacterial load and mitigate symptoms. However, patients must follow the prescribed course diligently and be aware of potential side effects to ensure optimal recovery and prevent complications.
At-Home Care and Remedies
Managing a wisdom tooth infection at home can help alleviate discomfort and control symptoms until you can seek professional dental care. One of the most effective methods is rinsing your mouth with a saltwater solution. Mixing half a teaspoon of salt into a glass of warm water and rinsing several times a day can help reduce inflammation and kill bacteria, providing temporary relief.
Over-the-counter pain relievers such as ibuprofen or acetaminophen can also be beneficial in managing the pain associated with a wisdom tooth infection. These medications can help reduce both pain and inflammation, making it easier to manage daily activities. Always follow the recommended dosage instructions on the packaging or consult with a pharmacist for advice.
Maintaining good oral hygiene is crucial when dealing with a wisdom tooth infection. Regular brushing and flossing can help prevent the infection from worsening. Consider using a toothbrush with soft bristles to avoid irritating the infected area further. Additionally, an antiseptic mouthwash may help keep the area clean and reduce bacterial growth.
Using a cold compress can also help manage swelling and pain. Applying an ice pack to the affected side of your face for 15-20 minutes at a time, several times a day, can provide a numbing effect and reduce inflammation. Be sure to wrap the ice pack in a cloth to protect your skin.
While these at-home remedies can offer temporary relief from the symptoms of a wisdom tooth infection, they are not a substitute for professional medical treatment. It is essential to consult with a dentist as soon as possible to address the underlying cause of the infection and receive appropriate care. Ignoring a wisdom tooth infection can lead to more severe complications and prolonged discomfort.
Preventive Measures
Preventing a wisdom tooth infection is paramount for maintaining optimal oral health. One of the most effective ways to reduce the risk is by scheduling regular dental check-ups. These visits allow your dentist to monitor the growth and position of your wisdom teeth, identifying potential issues before they escalate into infections. Early detection can significantly reduce the likelihood of complications and ensure timely intervention.
Proper oral hygiene practices are another cornerstone of prevention. Brushing and flossing daily, along with using an antiseptic mouthwash, can help keep harmful bacteria at bay. Since wisdom teeth are located at the back of the mouth, they are often harder to clean effectively. Special attention should be given to these areas to prevent food particles and plaque from accumulating, which can lead to infections.
Monitoring the growth and position of wisdom teeth is essential. Impacted wisdom teeth, which do not fully emerge through the gum line, are particularly prone to infections. Regular dental X-rays can provide a clear picture of how your wisdom teeth are developing and whether they pose any risk to your oral health. If they are likely to cause problems, your dentist may recommend preemptive removal.
Preemptive removal of wisdom teeth is a common strategy to avoid future complications. While not everyone needs to have their wisdom teeth extracted, it is often advisable for those whose teeth are impacted or growing at an angle. This proactive approach can prevent wisdom tooth infections and other related issues, such as damage to adjacent teeth or cyst formation.
In essence, a combination of regular dental visits, diligent oral hygiene, and careful monitoring can go a long way in preventing wisdom tooth infections. By taking these preventive measures seriously, you can preserve your oral health and avoid the discomfort and complications associated with wisdom tooth infections.
Conclusion and Final Thoughts
Wisdom tooth infections can pose significant health challenges if not addressed promptly. Recognizing the early symptoms, such as swelling, pain, and difficulty in opening the mouth, is crucial for timely intervention. Early diagnosis and treatment by a dental professional can prevent complications and alleviate discomfort swiftly.
Our discussion has highlighted several critical points about wisdom tooth infections. Firstly, these infections often stem from partially erupted wisdom teeth, which create an environment conducive to bacterial growth. Secondly, the importance of professional dental intervention cannot be overstated. Dentists can provide appropriate treatments, including antibiotics and surgical options, to manage the infection effectively.
Preventive measures play a pivotal role in mitigating the risk of wisdom tooth infections. Maintaining a rigorous oral hygiene routine, including regular brushing and flossing, helps in keeping bacterial build-up at bay. Additionally, routine dental check-ups are essential for monitoring the health of your wisdom teeth and identifying potential issues before they escalate.
In conclusion, understanding the nuances of wisdom tooth infections empowers individuals to take proactive steps towards their oral health. By staying vigilant about the symptoms, seeking timely professional care, and adhering to preventive practices, you can minimize the risks associated with these infections. Prioritizing oral health not only ensures a pain-free life but also contributes to overall well-being.
FAQs
-
What are the symptoms of wisdom tooth infection?
Wisdom tooth infections can be quite painful and may present with several symptoms. Common signs include severe pain around the tooth area, swelling in the gums, difficulty opening your mouth, and a bad taste in your mouth. In some cases, you might also experience fever and swollen lymph nodes. It’s important to recognize these symptoms early to prevent the infection from spreading.
-
Can wisdom tooth infections go away on their own?
While some mild cases of wisdom tooth infection may seem to improve on their own, it is generally not advisable to leave it untreated. Infections can worsen and lead to more serious complications if not addressed promptly. Over-the-counter pain relievers and saltwater rinses might provide temporary relief, but professional dental treatment is often necessary to fully resolve the infection.
-
How to Know if a Wisdom Tooth Hole is Infected?
After a wisdom tooth extraction, the site may be vulnerable to infection. Signs that the extraction site is infected include persistent pain, redness or swelling that worsens over time, and a discharge of pus. If you notice any of these symptoms, it’s crucial to contact your dentist immediately for an evaluation and appropriate treatment.
-
Is an Infected Wisdom Tooth an Emergency?
An infected wisdom tooth can indeed be considered a dental emergency, especially if it causes severe pain, fever, or difficulty swallowing or breathing. These symptoms suggest that the infection may be spreading, necessitating prompt medical attention. Delaying treatment can result in more complex health issues, so it’s essential to seek professional help as soon as possible.