Table of Contents
Introduction to Dental Extractions
Dental extractions are a common dental procedure that involves the removal of one or more teeth from the dental alveolus, or socket, in the alveolar bone. The necessity for dental extractions can arise from various conditions including severe tooth decay, periodontal disease, tooth fractures, or overcrowding of teeth.
When a tooth is damaged beyond repair, extraction becomes an essential step to prevent the spread of infection and maintain overall oral health. Additionally, extractions may be recommended prior to orthodontic treatments to facilitate proper alignment of the remaining teeth.
The process of performing a dental extraction requires careful consideration of several factors to ensure a successful outcome. One of the most critical aspects is the management of bone tissue damage. During the extraction, the surrounding bone can be compromised, which can have significant implications for the healing process and the future stability of the dental arch. Proper management of bone tissue is crucial to minimizing post-operative complications and promoting effective recovery.
Understanding the dynamics of bone tissue damage and implementing strategies to mitigate its impact are paramount. This involves employing advanced extraction techniques, utilizing appropriate tools, and considering adjunctive therapies to preserve bone integrity. The goal is not only to remove the problematic tooth but also to lay the groundwork for optimal healing and potential future dental restorations, such as implants or bridges.
In essence, dental extractions are more than just the removal of teeth; they are a complex procedure that necessitates a comprehensive approach to ensure the well-being of the patient. By prioritizing the management of bone tissue damage, dental professionals can significantly enhance patient outcomes, leading to faster recovery times and more predictable long-term results.
Understanding Bone Tissue Damage
During dental extractions, bone tissue damage is an inevitable concern that requires careful management to ensure optimal oral health outcomes. The jawbone, or alveolar bone, plays a critical role in supporting teeth, and any damage to this structure can have significant implications. The alveolar bone is part of the jaw that contains the tooth sockets. When a tooth is extracted, the surrounding bone and gum tissue can be affected, leading to potential complications.
There are several types of bone tissue damage that can occur during a dental extraction.
- One common type is the fracture of the alveolar bone, which can happen if the bone is brittle or if excessive force is applied during the extraction process.
- Another type of damage is bone resorption, where the bone tissue begins to break down and get absorbed into the body. This process can be accelerated after tooth extraction due to the loss of stimulation that the tooth once provided to the jawbone.
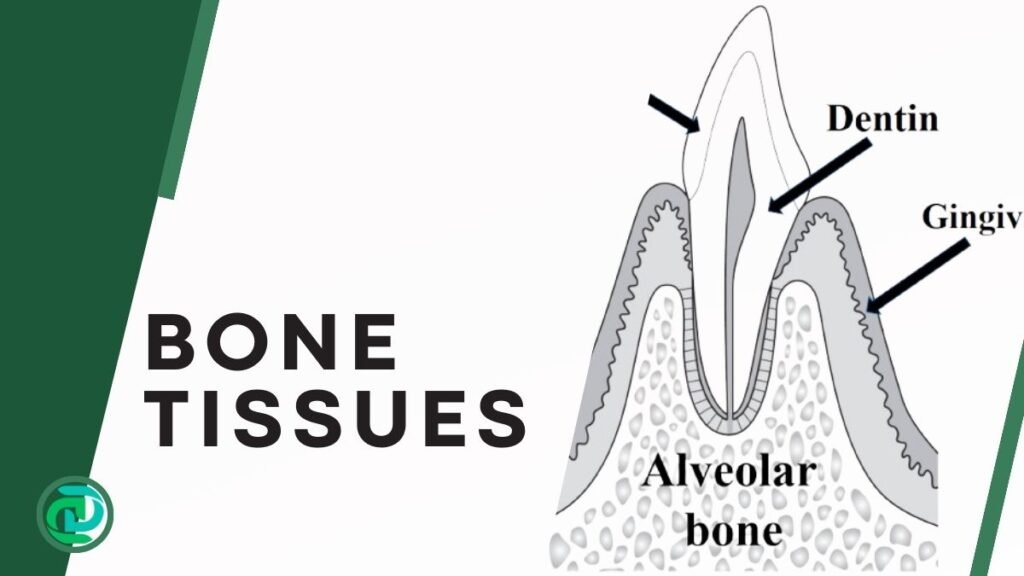
The implications of bone tissue damage are far-reaching. Without proper socket preservation techniques, the bone can deteriorate, leading to a loss of bone density and height. This can affect the overall structure and appearance of the jawline, potentially causing difficulties in fitting dental prosthetics like implants or dentures in the future. Additionally, bone resorption can lead to changes in facial aesthetics and impair the function of the remaining teeth.
Understanding the nature of bone tissue damage and its consequences is essential for both dental professionals and patients. Effective management strategies, such as bone grafting and the use of regenerative materials, can help mitigate these effects. By preserving the integrity of the alveolar bone, we can ensure better oral health outcomes and maintain the structural stability of the jawbone for future dental procedures.
Pre-Extraction Assessment
Before proceeding with a dental extraction, a comprehensive pre-extraction assessment is essential to evaluate the risk of bone tissue damage. This preliminary evaluation helps in planning the procedure meticulously and minimizing potential trauma to the bone tissue.
One of the critical components of this assessment is the use of diagnostic imaging tools such as X-rays and CT scans. These tools provide detailed images of the tooth, surrounding bone, and adjacent structures, allowing dental professionals to identify any potential complications that might arise during the extraction.
X-rays, particularly panoramic radiographs, offer a broad view of the entire mouth, revealing the condition of the bone and the positioning of the teeth. This diagnostic tool is invaluable in detecting any underlying issues such as bone defects, cysts, or impacted teeth that could complicate the extraction process. CT scans, on the other hand, provide three-dimensional images, offering a more detailed view of the bone and tooth structure. This advanced imaging technique is particularly useful in complex cases, enabling precise surgical planning and reducing the likelihood of inadvertent bone damage.

In addition to diagnostic imaging, a thorough patient health evaluation is conducted. This involves reviewing the patient’s medical history, current medications, and any underlying health conditions that might affect the healing process or increase the risk of complications.
Conditions such as osteoporosis, diabetes, or a history of bisphosphonate use can significantly impact bone health and the overall outcome of the extraction. Understanding these factors allows the dental professional to tailor the extraction procedure to the patient’s specific needs, employing strategies to protect the bone tissue.
Planning strategies to minimize trauma to the bone tissue are also an integral part of the pre-extraction assessment. This includes selecting the appropriate surgical technique, considering less invasive methods, and preparing for potential complications. By combining detailed diagnostic imaging with a thorough patient evaluation and strategic planning, the risk of bone tissue damage during a dental extraction can be significantly reduced, ensuring a smoother and safer procedure.
Techniques to Minimize Bone Tissue Damage
In the realm of dental extractions, minimizing bone tissue damage is paramount for ensuring optimal patient outcomes and facilitating faster recovery. Various surgical techniques and specialized tools have been developed to mitigate the risk of bone damage during tooth removal.
Atraumatic extraction methods are at the forefront of these advancements. These methods focus on preserving the integrity of the surrounding bone and soft tissues, thereby reducing postoperative complications.
One widely adopted technique is the application of periotomes, slender instruments designed to sever the periodontal ligament fibers without exerting excessive force on the alveolar bone. By carefully maneuvering periotomes around the tooth, dentists can effectively loosen it from the socket with minimal trauma.

Elevators also play a crucial role in atraumatic extractions. These tools come in various shapes and sizes, allowing for precise application of force to luxate the tooth gently. The use of elevators requires skill and precision to avoid undue pressure on the bone tissue. When used correctly, they can significantly decrease the likelihood of bone fractures and other complications.
Sectioning teeth is another technique that facilitates easier and less traumatic removal, particularly in cases of multi-rooted teeth or those with complex anatomy. By dividing the tooth into smaller sections, dentists can extract each piece individually, thereby reducing the amount of force needed and minimizing stress on the surrounding bone. This method is particularly beneficial for impacted teeth or those situated close to vital structures.

Collectively, these techniques underscore the importance of a meticulous and patient-centered approach in dental extractions. By utilizing atraumatic methods, periotomes, elevators, and tooth sectioning, dental professionals can significantly reduce the risk of bone tissue damage, enhance patient comfort, and expedite the healing process.
Management During Extraction
Effective management of bone tissue damage during dental extractions is paramount to ensuring optimal patient outcomes. One of the foremost strategies is the gentle handling of both hard and soft tissues. Using delicate and precise techniques minimizes unnecessary trauma and preserves the integrity of the bone. Employing instruments that are appropriately sized and designed for atraumatic extractions can significantly reduce the risk of bone fractures and splintering.
Maintaining excellent visual access to the surgical site is another crucial aspect. Adequate illumination and magnification tools, such as surgical loupes or microscopes, allow the dental practitioner to perform extractions with greater precision. Clear visibility helps in identifying vital anatomical structures and avoiding inadvertent damage. It also aids in the meticulous removal of tooth fragments and roots, which is essential to prevent post-operative complications.
The use of irrigation during extractions plays a vital role in mitigating bone tissue damage. Continuous irrigation with sterile saline or other appropriate solutions serves multiple purposes.
- Firstly, it reduces heat generation caused by the friction of dental instruments, thereby preventing thermal damage to the bone.
- Secondly, irrigation helps to flush out bone and tooth debris, maintaining a clean surgical field and reducing the risk of infection.
- Moreover, it can enhance the visibility of the operative area, allowing for more precise and controlled maneuvers.
Incorporating these intraoperative strategies is fundamental to managing bone tissue damage effectively during extractions. By prioritizing gentle handling, ensuring good visual access, and utilizing irrigation, dental professionals can significantly improve the prognosis and comfort for their patients. These measures not only facilitate smoother surgical procedures but also contribute to faster healing and reduced post-operative complications.
Post-Extraction Care and Bone Preservation
Effective management of bone tissue damage following dental extractions hinges on meticulous post-extraction care practices. These practices are essential in ensuring that the healing process is optimized, thereby promoting bone preservation and regeneration.
1. Socket Preservation
One of the primary techniques employed in this context is socket preservation. This process involves filling the extraction socket with graft material to prevent alveolar bone loss.
By maintaining the structure of the socket, the integrity of the bone is preserved, which is crucial for any future dental implants or prosthetic restorations.
2. Bone Grafts
In addition to socket preservation, bone grafts play a pivotal role in post-extraction care. Bone grafting materials, such as autografts, allografts, xenografts, and synthetic options, are utilized to augment the bone volume and promote new bone formation.

These materials act as scaffolds, facilitating the migration of osteogenic cells and the deposition of new bone matrix. The integration of bone grafts into the healing process not only supports the structural stability of the jaw but also enhances the overall aesthetic and functional outcomes of dental treatments.
3. Membrane barriers
Membrane barriers are another critical component in the management of bone tissue damage.
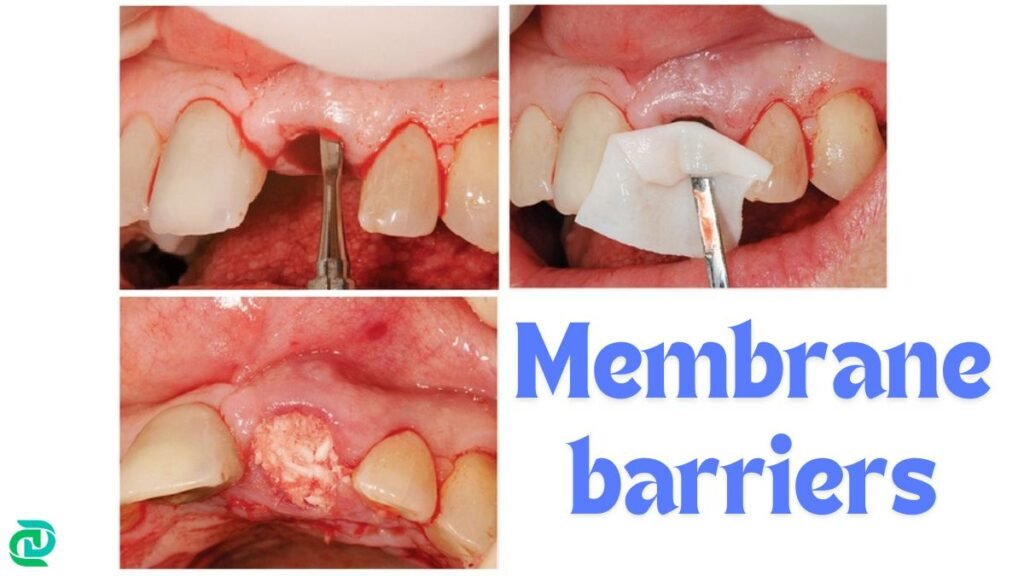
These barriers are used in conjunction with bone grafts to protect the graft material from soft tissue invasion, thus ensuring that the bone regeneration process occurs uninterrupted. By providing a secluded environment for osteogenesis, membrane barriers contribute significantly to the success of bone preservation efforts.
4. Medications
Medications also play a supportive role in promoting bone regeneration post-extraction. Pharmacological agents such as antibiotics, anti-inflammatory drugs, and bone morphogenetic proteins (BMPs) are often prescribed to mitigate infection, reduce inflammation, and stimulate bone growth, respectively.
The judicious use of these medications can enhance the body’s natural healing mechanisms, thus accelerating the recovery process and improving outcomes.
5. Diet
Dietary recommendations play a vital role in post-extraction recovery. Patients are advised to consume soft foods and avoid hot, spicy, or crunchy items that can irritate the extraction site. Staying hydrated is also important, but patients should avoid using straws, as the suction can dislodge the blood clot essential for healing.
6. Follow-up
Follow-up visits are crucial for monitoring the healing process. During these appointments, the dentist will check for any signs of complications and ensure that the recovery is progressing as expected. Patients should be aware of symptoms such as persistent pain, swelling, or bleeding, and report these to their dentist promptly.
In summary, the management of bone tissue damage in dental extractions requires a multifaceted approach. Through the integration of socket preservation techniques, bone grafts, membrane barriers, and medications, dental professionals can effectively promote bone healing and preservation, ensuring optimal long-term results for patients.
Complications and Their Management
Dental extractions, while routine, can sometimes lead to complications involving bone tissue damage.
1. Dry Socket
One of the most common complications is dry socket, also known as alveolar osteitis. This condition occurs when the blood clot at the site of extraction fails to form properly or dislodges prematurely, exposing the bone and nerves. Symptoms include severe pain, bad breath, and an unpleasant taste in the mouth.
Immediate management involves rinsing the socket with saline solution, applying medicated dressings, and prescribing pain relief medications.
2. Infection
Infection is another significant complication that can arise from bone tissue damage during dental extractions. Signs of infection include persistent pain, swelling, fever, and pus discharge. Early detection and intervention are crucial to prevent the infection from spreading.
Management typically involves the administration of antibiotics, thorough cleaning of the extraction site, and sometimes surgical debridement to remove necrotic tissue.
3. Bone Loss
Excessive bone loss is a less common but serious complication. It can lead to structural weaknesses and affect the overall stability of the jaw. Excessive bone loss can be identified through imaging techniques such as X-rays or CT scans.
Preventative measures include atraumatic extraction techniques, use of bone grafts, and immediate placement of dental implants to preserve the bone structure.
If bone loss is already present, regenerative procedures such as bone grafting or guided bone regeneration may be necessary to restore the lost tissue.
Preventing these complications involves a comprehensive preoperative assessment and meticulous surgical techniques. Patients should be thoroughly informed about post-operative care, including maintaining oral hygiene, avoiding smoking, and adhering to the prescribed medication regimen. Regular follow-up appointments are essential to monitor healing and address any emerging issues promptly.
Effective management of complications arising from bone tissue damage during dental extractions is pivotal for ensuring successful outcomes and patient satisfaction. By recognizing early signs and implementing appropriate interventions, dental professionals can mitigate risks and promote optimal healing.
Future Directions and Innovations
Emerging research in the management of bone tissue damage during dental extractions is paving the way for significant advancements in patient care. One of the most promising areas is the development of advanced biomaterials.
These materials, designed to be biocompatible and promote bone regeneration, are increasingly being utilized in dental procedures. Innovations like bioactive glass, hydroxyapatite composites, and bioresorbable polymers are showing great potential in enhancing bone healing post-extraction.
Tissue engineering is another frontier that holds considerable promise. By combining cells, growth factors, and scaffolds, tissue engineering aims to create functional bone tissue that can replace damaged areas. This approach not only accelerates the healing process but also ensures that the new bone integrates seamlessly with the existing tissue. Recent studies have demonstrated the efficacy of using stem cells derived from dental pulp or bone marrow, which can differentiate into osteoblasts and contribute to bone regeneration.
Minimally invasive techniques are also revolutionizing the field. Advances in technology have led to the development of tools and methods that reduce trauma to the bone tissue during extractions. For instance, piezoelectric surgery, which uses ultrasonic vibrations, allows for precise cutting with minimal damage to the surrounding bone and soft tissue. This technique not only reduces postoperative pain and swelling but also shortens recovery time.
Additionally, the integration of digital technologies, such as computer-aided design and manufacturing (CAD/CAM) and 3D printing, is transforming the landscape of dental surgery. These technologies enable the creation of precise surgical guides and custom implants that fit the patient’s anatomy perfectly, thereby improving the accuracy of the procedure and the overall outcome.
As research continues to evolve, these innovations are expected to become more refined and widely adopted, offering new horizons in the management of bone tissue damage in dental extractions. The future of dental surgery looks promising, with the potential for improved patient outcomes and enhanced quality of life.
Summary
In conclusion, a multifaceted approach that includes proper pre-extraction assessments, advanced surgical techniques, cutting-edge technology, and the expertise of the dentist is essential for minimizing bone tissue damage during dental extractions.
This holistic strategy not only enhances patient satisfaction but also contributes to faster recovery and better overall oral health.
FAQs
-
What is the management of bone tissue damage in dental extractions?
The best methods to manage bone tissue damage in dental extraction are: Socket Preservation, Bone Grafts, Membrane barriers, Medications, Diet, Follow-up visits.
-
How do you treat osteomyelitis after tooth extraction?
the comprehensive management of osteomyelitis post-extraction involves a combination of antibiotic therapy, surgical debridement, and potentially hyperbaric oxygen therapy. Each treatment plan must be individualized, taking into account the specifics of the infection and the overall health of the patient, to achieve the best possible outcomes.
-
How do you rebuild a bone after a tooth extraction?
Bone grafting is a widely used technique in which a bone graft material is placed in the extraction site to promote new bone growth. Autografts, allografts, xenografts, and synthetic bone graft.
-
What happens if you have bone loss after teeth extraction?
From a functional perspective, bone loss compromises the stability and retention of dental prosthetics such as dentures and implants. The diminished bone volume can make it challenging to place implants, necessitating additional procedures like bone grafting to rebuild the lost bone structure. Furthermore, the loss of bone density can lead to misalignment of the remaining teeth, contributing to further dental complications such as difficulty in chewing, speech impairments, and increased susceptibility to periodontal diseases.
-
How do you treat jawbone loss?
treating jaw bone loss requires a multi-faceted approach that combines surgical techniques, such as bone grafting and ridge augmentation, with non-surgical options like medications and lifestyle changes. This comprehensive strategy ensures optimal outcomes and long-term oral health for patients.
-
How do you fix osteonecrosis of the jaw?
The management of ONJ encompasses a range of strategies, from conservative approaches to surgical interventions. Conservative management typically involves the use of antibiotics to control infection, pain relief medications, and antiseptic mouth rinses. Soft diet recommendations and meticulous oral hygiene are also essential components of conservative care.