Table of Contents
Introduction to Pericoronitis
Pericoronitis is a dental condition characterized by the inflammation of the soft tissues surrounding a partially erupted tooth, most commonly a wisdom tooth. This inflammation typically occurs when the tooth does not fully emerge from the gum line, creating a flap of gum tissue that can easily trap food particles and bacteria. The resulting infection and swelling can lead to significant discomfort and, in severe cases, can make pericoronitis pain unbearable.
The primary causes of pericoronitis include poor oral hygiene, the presence of impacted wisdom teeth, and the accumulation of food debris under the gum flap. These factors contribute to an environment conducive to bacterial growth, leading to infection and inflammation. The typical symptoms of pericoronitis are swelling, redness, and tenderness of the affected gum tissue, along with difficulty in opening the mouth, bad breath, and an unpleasant taste in the mouth. In more severe cases, individuals may experience fever, swollen lymph nodes, and intense, persistent pain.
The pain associated with pericoronitis can become particularly unbearable due to the proximity of the affected area to numerous nerves in the jaw and face. The inflammation and infection can exert pressure on these nerves, amplifying the sensation of pain. Additionally, the constant irritation from chewing and speaking can exacerbate the discomfort, making daily activities challenging.
Understanding the underlying causes and symptoms of pericoronitis is crucial for effective management and treatment. Early diagnosis and proper oral hygiene practices can help mitigate the severity of the condition, reducing the likelihood of the pain becoming unbearable. For individuals experiencing significant discomfort, seeking prompt dental care is essential to alleviate symptoms and prevent further complications.
Symptoms and Diagnosis
Pericoronitis, particularly when severe, can manifest a range of distressing symptoms that significantly impact daily life. The most prominent of these symptoms is pericoronitis pain, often described as unbearable. This pain is typically localized around a partially erupted wisdom tooth and can radiate to adjacent areas, causing considerable discomfort.
Swelling is another common symptom. The gum tissue surrounding the affected tooth often becomes inflamed, leading to noticeable swelling in the jaw. This swelling can make it difficult to open the mouth fully, chew, or even speak. In some cases, the inflammation can spread to the cheek and throat, exacerbating the discomfort.
Difficulty swallowing, or dysphagia, is also frequently reported by those suffering from pericoronitis. The inflamed gums and surrounding tissues can create a sensation of obstruction in the throat, making it painful to swallow food or even liquids. Additionally, bad breath, or halitosis, is a common occurrence due to the accumulation of bacteria in the inflamed area, which can contribute to a foul taste in the mouth.
The impact of these symptoms on daily life can be profound. Individuals may find it challenging to maintain regular eating habits, leading to nutritional deficiencies. The persistent pain and discomfort can interfere with sleep, work, and social interactions, diminishing overall quality of life.
Diagnosing pericoronitis requires a thorough examination by a dental professional. The process typically begins with a detailed medical history and a physical examination of the mouth. The dentist will look for signs of inflammation, swelling, and tenderness around the partially erupted tooth. In some cases, imaging tests such as X-rays may be necessary to assess the position of the wisdom tooth and the extent of the infection. These diagnostic tools help to confirm the presence of pericoronitis and rule out other potential causes of the symptoms.
Causes and Risk Factors
Pericoronitis, a condition often characterized by unbearable pain, primarily arises from bacterial infections. These infections typically occur when food particles and debris become trapped beneath the gum flap covering a partially erupted tooth, commonly a wisdom tooth. The warm, moist environment under the gum flap becomes an ideal breeding ground for bacteria, leading to inflammation and infection.
- Poor oral hygiene significantly increases the risk of developing pericoronitis. Inadequate brushing and flossing allow plaque and food particles to accumulate, exacerbating the problem. Regular dental check-ups and professional cleanings are essential preventive measures, as they help remove plaque buildup and detect potential issues early.
- Partially erupted teeth, particularly wisdom teeth, are another major risk factor. These teeth often lack sufficient space to fully emerge, causing them to become partially covered by a gum flap. This partial eruption creates a pocket where bacteria and debris can easily accumulate, leading to infection. Furthermore, the pressure from partially erupted teeth can also cause discomfort and pain, making the situation even more challenging.
- The age group most commonly affected by pericoronitis is young adults, typically between the ages of 17 and 25. This is the period when wisdom teeth usually begin to emerge. During this time, individuals are more susceptible to the condition due to the common occurrence of partially erupted teeth. However, it is important to note that pericoronitis can affect individuals outside this age range, especially if they experience similar dental issues.
- Other contributing factors include a weakened immune system, which can make it harder for the body to fight off infections, and certain lifestyle choices, such as smoking or a diet high in sugary foods, which can promote bacterial growth. Recognizing these causes and risk factors is crucial in understanding how to manage and prevent the unbearable pain associated with pericoronitis.
Immediate Relief Strategies
When dealing with pericoronitis pain that seems unbearable, immediate relief strategies can prove invaluable. One of the most accessible methods is the use of over-the-counter pain medications. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or aspirin can help reduce inflammation and alleviate discomfort. It is crucial to adhere to the recommended dosages to avoid potential side effects.
Another effective home remedy involves saltwater rinses. Dissolving a teaspoon of salt in a glass of warm water and gently rinsing the mouth multiple times a day can help decrease swelling and cleanse the affected area. This practice not only provides temporary relief but also aids in maintaining oral hygiene, which is vital during periods of intense pain.
Cold compresses are an additional strategy for managing unbearable pericoronitis pain. Applying a cold pack to the outside of the cheek near the affected area can numb the pain and reduce swelling. It is advisable to wrap the cold pack in a cloth to prevent direct skin contact, and to limit application to 15-20 minute intervals.
Maintaining oral hygiene, even when in pain, is crucial to prevent further complications. Brushing gently around the affected area with a soft-bristled toothbrush and using an antiseptic mouthwash can help keep bacteria at bay. However, care must be taken not to aggravate the inflamed tissue further.
Moreover, certain foods should be avoided as they can worsen the condition. Hard, crunchy, or spicy foods may irritate the inflamed gums, while sugary foods can promote bacterial growth. Opting for soft, bland foods can minimize discomfort and lower the risk of exacerbating the pain.
Implementing these immediate relief strategies can significantly ease the unbearable pain of pericoronitis, allowing for better management until professional dental care can be sought.
Professional Treatment Options
When pericoronitis pain becomes unbearable, seeking professional treatment is often necessary to alleviate discomfort and prevent further complications. Several treatment options are available, each with its own set of benefits and risks. Understanding these options is crucial for making informed decisions about your oral health.
One common treatment for pericoronitis is the administration of antibiotics. This approach is particularly effective when the pain is caused by a bacterial infection. Antibiotics can help reduce inflammation and eliminate the infection, providing relief from the unbearable pain associated with pericoronitis. However, it is important to complete the entire course of antibiotics as prescribed to ensure the infection is fully eradicated. Overuse or misuse of antibiotics can lead to antibiotic resistance, making future treatments more challenging.
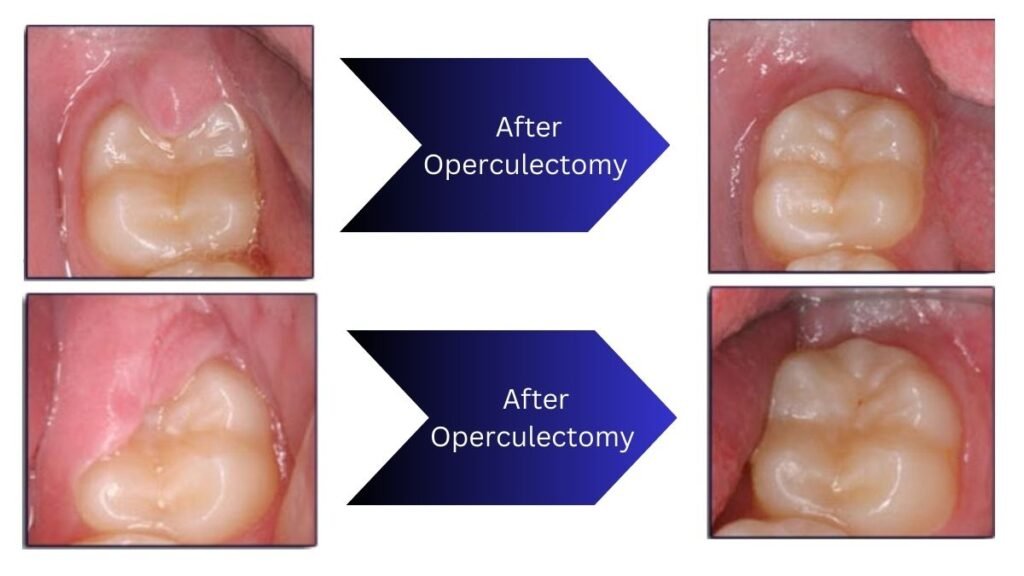
In some cases, a minor surgical procedure called an operculectomy may be recommended. This involves removing the gum flap that covers the partially erupted tooth, thereby eliminating the source of irritation and infection. The benefits of this procedure include immediate relief from pain and a decreased risk of future infections. However, like any surgical intervention, there are risks involved, such as bleeding, infection, and discomfort during the healing process.
For more severe cases of pericoronitis, especially when the tooth is impacted or causing significant problems, extraction of the affected tooth may be necessary. Tooth extraction can provide a permanent solution to the issue, preventing further episodes of pericoronitis pain. The primary benefit of this approach is the complete eradication of the problem tooth, which can offer long-term relief. Nevertheless, tooth extraction is a more invasive procedure and carries risks such as infection, prolonged bleeding, and potential damage to adjacent teeth or nerves.
Consulting with a dental professional is essential for determining the most appropriate treatment option based on the severity of the condition and individual patient factors. Each treatment carries its own set of considerations, and a tailored approach will ensure optimal outcomes for those suffering from pericoronitis pain.
Preventive Measures
Preventing pericoronitis, a condition often associated with unbearable pain, requires a proactive approach to oral hygiene and lifestyle habits. Ensuring meticulous oral hygiene is paramount. This includes brushing teeth at least twice a day with fluoride toothpaste and using dental floss to remove food particles and plaque from between the teeth. Special attention should be given to the area around partially erupted teeth, as these are particularly susceptible to bacterial buildup.
Regular dental check-ups play a crucial role in detecting early signs of pericoronitis. Dentists can identify potential problem areas and provide professional cleanings to remove any plaque or tartar that has accumulated. They can also offer guidance on how to properly clean hard-to-reach areas, particularly around wisdom teeth that have not fully erupted.
Proper cleaning techniques are essential in preventing pericoronitis. Using an antiseptic mouthwash can help reduce bacteria in the mouth, thereby lowering the risk of infection. Additionally, investing in a water flosser can aid in cleaning around partially erupted teeth more effectively than traditional flossing alone.
Lifestyle changes can also play a significant role in reducing the risk of pericoronitis. A diet low in sugar and high in fiber helps maintain overall oral health. Sugary foods and drinks can promote the growth of bacteria, leading to infections. On the other hand, a balanced diet rich in fruits and vegetables supports gum health and can help prevent the onset of pericoronitis.
Finally, avoiding tobacco and moderating alcohol consumption are critical steps in maintaining oral health and reducing the risk of infections, including pericoronitis. Tobacco and alcohol can weaken the immune system and dry out the mouth, creating an environment where bacteria can thrive. By adopting these preventive measures, individuals can significantly lower the chances of experiencing the unbearable pain associated with pericoronitis.
When to See a Dentist
Pericoronitis is a condition that can cause significant discomfort, often leading individuals to seek medical attention. Recognizing the signs and symptoms that necessitate professional dental care is crucial in managing pericoronitis pain, which can sometimes become unbearable. If you experience severe pain, swelling, or difficulty opening your mouth, it is essential to consult a dentist promptly. Additional symptoms such as a foul taste in the mouth, bad breath, or a fever indicate that the infection may be spreading, requiring immediate intervention.
Early intervention by a dental professional can prevent complications such as abscess formation or the spread of infection to adjacent tissues. Dentists are equipped to diagnose pericoronitis accurately and offer effective treatment options, which may include thorough cleaning of the affected area, pain management strategies, and sometimes minor surgical procedures to alleviate the condition.
During a dental visit for pericoronitis, you can expect a comprehensive examination of your mouth. The dentist will likely take X-rays to assess the position of the wisdom teeth and the extent of the infection. Based on their findings, they will discuss a tailored treatment plan with you. This plan may involve the use of antibiotics to control the infection, pain relief medications, and instructions for maintaining proper oral hygiene to prevent recurrence.
Preparation for a dental visit involves gathering relevant medical history, including any medications you are currently taking, and noting any allergies. It is also helpful to write down the symptoms you are experiencing and any questions you may have for the dentist. This preparation ensures a more efficient and effective consultation, allowing the dentist to provide the best possible care for your pericoronitis pain, which can often feel unbearable.
Living with Pericoronitis
Living with pericoronitis can be an arduous experience, particularly when the pericoronitis pain becomes unbearable. For many individuals, managing this condition requires a multifaceted approach that addresses both the physical and psychological aspects of the ailment. During flare-ups, implementing effective pain management strategies is crucial. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help mitigate the discomfort. Additionally, maintaining rigorous oral hygiene practices, including thorough brushing and flossing around the affected area, can reduce inflammation and prevent secondary infections.
Long-term care for pericoronitis involves ongoing monitoring and possible lifestyle adjustments. Regular dental check-ups are essential to catch any early signs of complications. Dentists may recommend the extraction of partially erupted wisdom teeth to eliminate the source of irritation and prevent future episodes. In some cases, more conservative treatments, such as antiseptic mouthwashes or saltwater rinses, can provide relief and reduce bacterial load.
It’s also important to consider the mental health implications of living with chronic pericoronitis. Persistent pain and discomfort can lead to anxiety and stress, which in turn can exacerbate the physical symptoms. Engaging in stress-reducing activities, such as yoga, meditation, or even talking to a mental health professional, can be beneficial. Support groups, either online or in-person, offer a platform to share experiences and coping strategies, helping individuals feel less isolated in their struggle.
Personal stories often provide valuable insights and hope. For instance, Sarah, a 28-year-old from Chicago, shares her journey of managing pericoronitis pain. “At first, the pain was unbearable, and I felt like it controlled my life. But through regular dental visits, a strict oral hygiene routine, and joining a support group, I found ways to cope and even thrive.” Such testimonials underscore the importance of a comprehensive approach to managing this condition, highlighting that with the right strategies, it is possible to lead a fulfilling life despite the challenges posed by pericoronitis.
FAQs
-
How to Stop Pericoronitis from Hurting?
One of the primary concerns for those suffering from pericoronitis is the pain associated with it. To alleviate this pain, you can rinse your mouth with warm salt water several times a day. Over-the-counter pain relievers like ibuprofen can also help reduce inflammation and pain. Maintaining good oral hygiene by gently brushing the affected area can prevent further infection.
-
How to Get Rid of Gum Pain from Wisdom Teeth?
Gum pain from wisdom teeth can be particularly bothersome. Besides using salt water rinses and pain relievers, applying a cold compress to the outside of your cheek can help reduce swelling and numb the pain. Avoiding hard or chewy foods that can aggravate the area is also advisable. If the pain persists, it is crucial to consult a dentist for further evaluation and treatment.
-
Can Pericoronitis Resolve Itself?
While mild cases of pericoronitis can sometimes resolve on their own with proper care, it is not guaranteed. Continuous monitoring and maintaining oral hygiene are vital. If the symptoms do not improve or worsen, professional dental intervention may be necessary to prevent complications.
-
Is Pericoronitis an Emergency?
Pericoronitis can become an emergency if left untreated, especially if it leads to severe infection or swelling that affects breathing or swallowing. If you experience such symptoms, seek immediate medical attention. Early treatment can prevent the condition from escalating to an emergency level.