Table of Contents
Introduction
Periodontal disease, also known as gum disease, is a prevalent oral health condition that affects millions of people worldwide.
It is often referred to as a silent epidemic because it can go unnoticed in its early stages and gradually progress, causing significant damage to the gums and supporting structures of the teeth.
In this article, we will explore the definition of periodontal disease and its significance in oral health. We will also discuss its prevalence and the impact it can have on the quality of life of those affected.
Understanding Periodontal Disease
The periodontium refers to the tissues that surround and support the teeth, including the gums, periodontal ligament, cementum, and alveolar bone.
Periodontal disease is a term used to describe a group of inflammatory conditions that affect these tissues. The two main forms of periodontal infection are gingivitis and periodontitis.
Anatomy of the Periodontium
The periodontium is a complex structure that plays a vital role in maintaining the health and stability of the teeth. It consists of several components:
- Gums (Gingiva): The gums are the soft tissues that cover the jawbone and surround the base of the teeth. They provide a protective barrier against bacteria and help support the teeth.
- Periodontal Ligament: The periodontal ligament is a fibrous connective tissue that connects the teeth to the surrounding bone. It acts as a shock absorber, allowing the teeth to withstand the forces of chewing and biting.
- Cementum: Cementum is a thin layer of hard tissue that covers the root surface of the teeth. It helps anchor the teeth to the jawbone and provides a surface for the attachment of the periodontal ligament.
- Alveolar Bone: The alveolar bone is the part of the jawbone that surrounds and supports the teeth. It provides a stable foundation for the teeth and is essential for maintaining their position in the mouth.
Gingivitis vs. Periodontitis
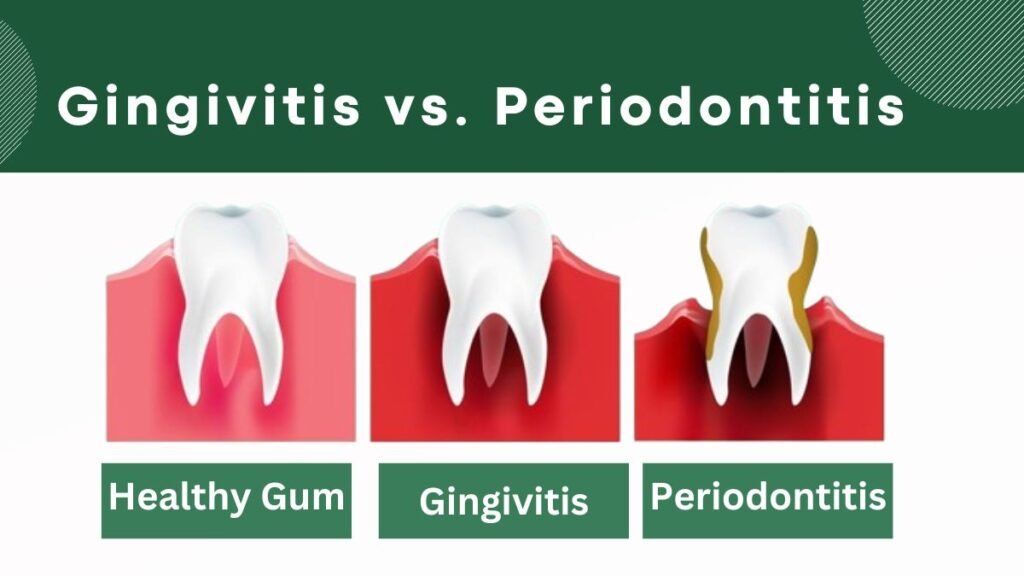
Gingivitis is the mildest form of periodontal disease and is characterized by inflammation of the gums. It is usually caused by the buildup of plaque, a sticky film of bacteria that forms on the teeth. If left untreated, gingivitis can progress to periodontitis.
Periodontitis is a more advanced form of periodontal infection that affects not only the gums but also the supporting structures of the teeth.
It occurs when the inflammation spreads below the gum line and leads to the destruction of the periodontal ligament and alveolar bone. Without proper treatment, periodontitis can result in tooth loss.
It is important to note that gingivitis can be reversed with proper oral hygiene and professional dental care. However, once periodontitis sets in, it requires more extensive treatment to manage and control the disease.
Causes and Risk
The primary cause of periodontal disease is the bacterial biofilm, commonly known as plaque, that accumulates on the teeth and gum line.
Plaque is a sticky film that forms when bacteria in the mouth combine with saliva and food particles.
If not removed through proper oral hygiene practices such as brushing and flossing, plaque can harden into tartar, which cannot be removed by regular brushing alone.
In addition to plaque, there are several other risk factors that can contribute to the development of periodontal infection:
- Smoking: Smoking is a significant risk factor for periodontal disease. It weakens the immune system, making it harder for the body to fight off infections, including those that affect the gums.
- Diabetes: Individuals with diabetes are at a higher risk of developing periodontal disease. Poorly controlled blood sugar levels can impair the body’s ability to heal and fight off infections.
- Genetics: Some individuals may be genetically predisposed to periodontal disease. Certain genetic variations can make it easier for bacteria to cause gum inflammation and damage.
- Hormonal changes: Hormonal changes that occur during puberty, pregnancy, and menopause can make the gums more susceptible to periodontal infection.
- Poor oral hygiene: Inadequate brushing and flossing can lead to the buildup of plaque and tartar, increasing the risk of gum disease.
- Stress: Chronic stress can weaken the immune system and make it harder for the body to fight off infections, including those that affect the gums.
- Poor nutrition: A diet lacking in essential nutrients can weaken the immune system and make it harder for the body to fight off infections.
Symptoms
Periodontal disease can manifest through various symptoms, and early detection is crucial for effective treatment. Some common symptoms include:
- Bleeding gums: One of the most common signs of gum disease is bleeding gums, especially during brushing or flossing. Healthy gums should not bleed.
- Bad breath: Persistent bad breath, also known as halitosis, can be a sign of periodontal infection. The bacteria in plaque release toxins that can cause an unpleasant odor.
- Red, swollen, or tender gums: Inflammation of the gums is a typical symptom of periodontal disease. The gums may appear red, swollen, or feel tender to the touch.
- Receding gums: As periodontal infection progresses, the gums may start to recede, making the teeth appear longer. This can also lead to tooth sensitivity.
- Loose or shifting teeth: Advanced periodontal infection can cause the teeth to become loose or shift in position. This can affect the bite and overall oral function.
If you experience any of these symptoms, it is important to seek professional dental care for a proper diagnosis. A dentist or periodontist will perform a thorough examination to assess the health of your gums and teeth.
Diagnosis
The professional diagnostic process for periodontal disease typically includes:
- Probing: The dentist or periodontist will use a probe to measure the depth of the spaces, or pockets, between the gums and teeth. Deeper pockets can indicate the presence of gum disease.
- X-rays: X-rays may be taken to assess the health of the underlying bone structure and identify any bone loss caused by periodontal disease.
- Dental history: The dentist will inquire about your dental history, including any previous diagnoses or treatments related to periodontal infection.
- Medical history: Information about your overall health, including any medical conditions or medications, will be considered as they can impact the health of your gums.
Based on the findings from the examination and diagnostic tests, the dentist or periodontist will determine the severity and extent of the periodontal infection. This information will guide the development of an appropriate treatment plan to address the specific needs of the individual.
The Stages of Periodontal Disease
Understanding the stages of periodontal infection is crucial for early detection and effective treatment. In this article, we will detail the progression from gingivitis to advanced periodontitis.
1. Gingivitis
Gingivitis is the initial stage of periodontal disease. It is characterized by inflammation of the gums caused by the accumulation of plaque, a sticky film of bacteria that forms on the teeth.
Common symptoms of gingivitis include red, swollen, and bleeding gums. However, gingivitis can be easily reversed with proper oral hygiene practices, such as regular brushing, flossing, and professional dental cleanings.
2. Early Periodontitis
If gingivitis is left untreated, it can progress to early periodontitis. At this stage, the inflammation extends beyond the gum line and affects the supporting structures of the teeth, including the bone and connective tissues.
Symptoms of early periodontitis may include persistent bad breath, receding gums, and the formation of periodontal pockets, which are spaces between the teeth and gums.
Treatment at this stage typically involves non-surgical interventions to remove plaque and tartar buildup, such as scaling and root planing.
3. Moderate to Advanced Periodontitis
If early periodontitis is not effectively treated, it can advance to moderate to advanced periodontitis.
In this stage, the damage to the supporting structures of the teeth becomes more severe, leading to tooth mobility, abscess formation, and potential tooth loss. The periodontal pockets deepen, allowing bacteria to thrive and further damage the tissues.
Treatment for moderate to advanced periodontitis may involve both non-surgical and surgical interventions, depending on the severity of the condition.
Classification System for Periodontal Diseases
To effectively diagnose and treat periodontal diseases, dental professionals use a classification system that helps categorize the different types and stages of the disease.
The most commonly used classification system is the one developed by the American Academy of Periodontology (AAP). This system provides a framework for understanding the extent and severity of periodontal diseases.
The AAP classification system categorizes periodontal infection into the following main groups:
1. Gingival Diseases
Gingival diseases are limited to the gums and do not involve the supporting structures of the teeth. These include conditions such as gingivitis and certain forms of periodontal abscesses.
Gingival diseases can usually be reversed with proper oral hygiene practices and professional dental care.
2. Chronic Periodontitis
Chronic periodontitis is the most common form of periodontal disease. It is characterized by the progressive inflammation and destruction of the supporting structures of the teeth.
This form of periodontitis can occur in both localized and generalized patterns and usually progresses slowly over time. Treatment for chronic periodontitis may involve non-surgical and surgical interventions, depending on the severity of the disease.
3. Aggressive Periodontitis
Aggressive periodontitis is a less common but more aggressive form of periodontal disease. It typically affects young individuals and is characterized by rapid bone destruction and tooth loss. Aggressive periodontitis can be localized, affecting specific teeth, or generalized, affecting the entire mouth.
Treatment for aggressive periodontitis often requires a combination of non-surgical and surgical approaches.
4.Necrotizing Periodontal Diseases
Necrotizing periodontal diseases are characterized by the death of gum tissues, leading to the formation of craters in the gums. These conditions are often associated with systemic factors, such as immune system disorders or smoking.
Treatment for necrotizing periodontal diseases involves a combination of professional dental care and addressing the underlying systemic factors.
Treatment Modalities for Periodontal Disease
The treatment of periodontal disease aims to control the infection, reduce inflammation, and prevent further damage to the supporting structures of the teeth.
Depending on the stage and severity of the disease, different treatment modalities may be recommended. In this section, we will explore non-surgical options like scaling and root planing, as well as surgical treatments, including flap surgery and bone grafts.
Non-Surgical Treatment
Non-surgical treatment options are often the first line of defense against periodontal disease. These treatments focus on removing the bacterial plaque and calculus (tartar) that accumulate on the teeth and below the gum line.
The most common non-surgical treatment for periodontal disease is scaling and root planing.
Scaling involves the removal of plaque and tartar from the tooth surfaces and the root surfaces below the gum line. This is usually performed using handheld instruments or ultrasonic scalers.
Root planing, on the other hand, involves smoothing the root surfaces to remove any rough areas that can harbor bacteria and contribute to further inflammation.
In addition to scaling and root planing, other non-surgical treatment modalities may be recommended depending on the individual case.
These include the use of antimicrobial mouth rinses, locally applied antibiotics, and host modulation therapy, which aims to modify the body’s immune response to control the progression of the disease.
Surgical Treatment
In cases where non-surgical treatments are not sufficient or the disease has progressed to an advanced stage, surgical interventions may be necessary.
Surgical treatments for periodontal disease aim to reduce pocket depths, regenerate lost bone and tissue, and improve the overall health and function of the gums.
One common surgical procedure for periodontal disease is flap surgery, also known as pocket reduction surgery.
During this procedure, the gums are lifted to expose the roots of the teeth and remove any plaque and tartar buildup. The underlying bone may also be reshaped to eliminate irregularities and create a more favorable environment for healing.
In cases where significant bone loss has occurred, bone grafts or regenerative procedures may be recommended. These procedures involve the placement of grafting materials, such as synthetic bone or bone from another part of the body, to stimulate the regeneration of lost bone and tissue.
Prevention and Maintenance
with proper prevention and maintenance, the risk of developing periodontal disease can be significantly reduced.
1. Emphasizing the Importance of Oral Hygiene
One of the most effective ways to prevent periodontal infection is by practicing good oral hygiene. This includes brushing your teeth at least twice a day with a fluoride toothpaste, flossing daily to remove plaque from between the teeth, and using an antimicrobial mouthwash to kill bacteria.
Additionally, it is important to replace your toothbrush every three to four months or sooner if the bristles become frayed. This ensures that you are using an effective tool for removing plaque and bacteria from your teeth.
2. Regular Dental Visits
In addition to maintaining a good oral hygiene routine at home, regular dental visits are essential for preventing periodontal-disease. Dentists and dental hygienists have the expertise and tools to thoroughly clean your teeth and gums, removing any plaque and tartar that may have accumulated.
During these visits, your dentist will also perform a comprehensive examination of your oral health, checking for any signs of periodontal-disease or other dental issues. Early detection is key in preventing the progression of periodontal-disease and avoiding potential complications.
3. Lifestyle Modifications to Reduce the Risk
Aside from oral hygiene and regular dental visits, certain lifestyle modifications can help reduce the risk of developing periodontal-disease. These include:
- Quitting smoking: Smoking is a significant risk factor for periodontal-disease. By quitting smoking, you can greatly improve your oral health and reduce the likelihood of developing periodontal infection.
- Eating a balanced diet: A diet rich in fruits, vegetables, and whole grains can help support a healthy immune system, which plays a crucial role in fighting off infections, including gum infections.
- Limiting sugary foods and beverages: Consuming excessive amounts of sugary foods and drinks can contribute to the development of plaque and increase the risk of periodontal infection. Limiting your intake of these items can help protect your oral health.
- Managing stress: Chronic stress can weaken the immune system and make you more susceptible to infections, including periodontal infection. Finding healthy ways to manage stress, such as exercise, meditation, or hobbies, can benefit your overall health, including your oral health.
Complications and Systemic Links
Periodontal disease is not just limited to the oral cavity. Research has shown a strong association between periodontal infection and various systemic health issues.
The link between oral health and overall health is becoming increasingly evident, highlighting the importance of maintaining good oral hygiene and seeking timely treatment for periodontal infection.
Association with Systemic Health Issues
Several systemic health issues have been linked to periodontal infection, including:
- Cardiovascular disease: Studies have found that individuals with periodontal infection are at a higher risk of developing heart disease and experiencing cardiovascular events such as heart attacks and strokes.
- Diabetes: gum disease can make it more difficult for individuals with diabetes to control their blood sugar levels. Conversely, uncontrolled diabetes can worsen periodontal infection.
- Respiratory infections: The bacteria present in the mouth can be inhaled into the lungs, potentially leading to respiratory infections such as pneumonia.
- Pregnancy complications: Pregnant women with gum disease may have an increased risk of preterm birth and low birth weight babies.
Potential Complications if Left Untreated
If left untreated, periodontal disease can lead to various complications, including:
- Gum recession: As the infection progresses, the gums may start to recede, exposing the tooth roots and making them more susceptible to decay and sensitivity.
- Bone loss: Advanced gum disease can cause the destruction of the bone supporting the teeth, leading to tooth loss.
- Tooth loss: When the supporting structures of the teeth are compromised, tooth loss can occur. This can significantly impact a person’s ability to chew, speak, and smile confidently.
- Chronic bad breath: The bacteria associated with periodontal infection can cause persistent bad breath, even after brushing and using mouthwash.
Advancements in Periodontal Care
Advancements in periodontal care have revolutionized the treatment and management of periodontal disease. These advancements aim to improve the effectiveness of treatment, enhance patient comfort, and promote better long-term outcomes.
Minimally Invasive Treatment Approaches
One notable advancement is the development of minimally invasive treatment approaches. Traditional periodontal surgery involved making incisions and suturing the gums, which could be uncomfortable and require a lengthy recovery period.
Nowadays, techniques such as laser therapy and minimally invasive surgery allow for targeted treatment of the affected areas with minimal disruption to the surrounding tissues. These approaches often result in less post-operative discomfort and faster healing times.
Regenerative Therapies
Regenerative therapies have also shown promise in the field of periodontal care. These therapies aim to restore the damaged tissues and bone caused by periodontal disease.
One example is the use of growth factors and specialized proteins to stimulate the regeneration of bone and connective tissue. This can help reverse the effects of bone loss and promote the reattachment of the gums to the teeth.
Future Directions and Potential Therapies
The field of periodontal care is continuously evolving, with ongoing research and development of new therapies. Some potential future directions in the treatment of periodontal disease include:
- Gene therapy: Researchers are exploring the use of gene therapy to target and modify the genes responsible for the development and progression of periodontal disease.
- Tissue engineering: Tissue engineering approaches aim to create new tissues, such as bone and gum tissue, to replace the damaged structures caused by periodontal disease.
- Microbiome modulation: The oral microbiome plays a crucial role in the development of periodontal infection. Modulating the microbiome through targeted interventions could offer new avenues for prevention and treatment.
While these potential therapies are still in the early stages of research, they hold promise for the future of periodontal care.
Summary
Periodontal disease is a common oral health condition that can have serious consequences if left untreated.
By understanding the causes, recognizing the symptoms, and seeking appropriate treatment, you can effectively manage periodontal disease and maintain good oral health.
Remember to prioritize oral hygiene practices, make necessary lifestyle changes, and consult with your dentist regularly to prevent and address any signs of gum disease.
FAQs
-
What is Periodontal Disease?
Periodontal disease, also known as gum disease, is a common oral health condition that affects the gums and supporting structures of the teeth. It is caused by bacteria in the mouth that can lead to inflammation and infection.
-
What are the Symptoms of Periodontal Disease?
The symptoms can vary depending on the stage of the condition. In the early stages, symptoms may include red, swollen, or tender gums, as well as bleeding during brushing or flossing. As the disease progresses, symptoms may include bad breath, receding gums, loose teeth, and changes in the way your teeth fit together when you bite.
-
What Causes Periodontal Disease?
Periodontal disease is primarily caused by the buildup of plaque, a sticky film of bacteria that forms on the teeth. When plaque is not removed through regular brushing and flossing, it hardens into tartar, which can only be removed by a dental professional. The bacteria in plaque and tartar release toxins that irritate the gums and cause inflammation, leading to periodontal disease.
-
How is Periodontal Disease Diagnosed?
Periodontal disease is diagnosed through a comprehensive dental examination. During the examination, the dentist or periodontist will visually inspect the gums, measure the depth of the pockets around the teeth, and may take dental X-rays to assess the extent of the disease. They may also perform a periodontal probing, which involves using a small instrument to measure the depth of the pockets and check for any signs of infection or inflammation.
-
What are the Treatment Options for Periodontal Disease?
The treatment depends on the severity of the condition. In the early stages, treatment may involve professional dental cleanings to remove plaque and tartar, as well as improved oral hygiene practices at home. In more advanced cases, treatments may include scaling and root planing, which involves deep cleaning of the root surfaces to remove bacteria and smooth out rough areas, or periodontal surgery to repair damaged gum tissue and bone.