Table of Contents
Introduction to Apicoectomy
An apicoectomy, also known as root-end surgery, is a specialized dental procedure aimed at preserving a tooth that has not responded to conventional endodontic treatments such as root canal therapy. This surgical intervention involves the removal of the apex, or tip, of a tooth’s root, along with any surrounding infected tissue. The primary goal is to eliminate the source of infection and inflammation, thereby facilitating healing and maintaining the tooth’s functionality.
In the realm of dental health, an apicoectomy is particularly significant for its role in addressing persistent or recurrent infections that cannot be resolved through standard root canal procedures. It is often recommended in situations where the root canal therapy has failed, or where anatomical complexities such as root fractures or calcifications impede conventional treatment methods. Additionally, it becomes a viable option when previous root canals have been performed but symptoms persist, indicating a deeper underlying issue that needs surgical intervention.
Typically, an apicoectomy is advised when other less invasive treatments have proven ineffective. For instance, when a patient continues to experience pain or signs of infection despite having undergone one or more root canal treatments, an apicoectomy may be necessary. It is also recommended in cases where an obstruction or unusual root anatomy makes it impossible to carry out further root canal work. By directly targeting the root apex and any problematic tissues, an apicoectomy can effectively resolve issues that are otherwise inaccessible through non-surgical means.
Understanding the apicoectomy success rate is crucial for patients considering this procedure. Numerous factors contribute to the likelihood of a successful outcome, including the skill of the dental surgeon, the location and condition of the tooth, and the patient’s overall health and oral hygiene. With a thorough grasp of what an apicoectomy entails and the contexts in which it is performed, patients can make informed decisions about their dental treatment options.
Procedure Overview
An apicoectomy is a surgical procedure aimed at removing the tip of a tooth’s root, along with any surrounding infected tissue. This procedure is typically recommended when a standard root canal treatment fails to eradicate the infection. Understanding the detailed steps involved can demystify the process and provide insights into the apicoectomy success rate.
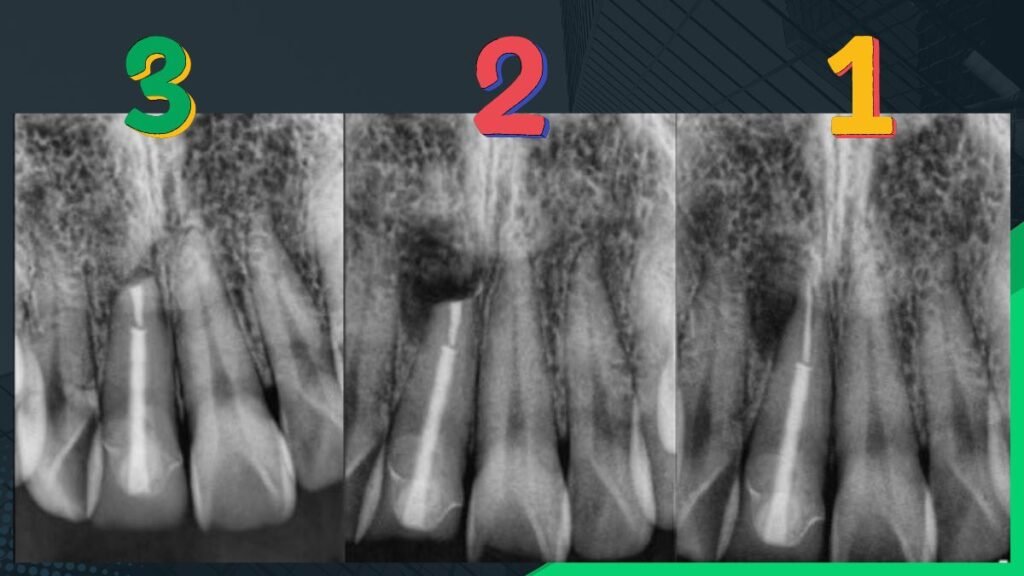
Preparation for an apicoectomy begins with a thorough dental examination, including X-rays to assess the extent of the infection and the structure of the tooth. The dentist or oral surgeon will discuss the procedure, potential risks, and benefits with the patient. Local anesthesia is administered to numb the area, ensuring that the patient is comfortable and experiences no pain during the surgery.
The surgical steps of an apicoectomy are precise and methodical. First, an incision is made in the gum tissue near the affected tooth to expose the underlying bone and root tip. Using specialized tools, the surgeon carefully removes the infected tissue and the tip of the root. The area is then cleaned and disinfected to eliminate any lingering bacteria. Occasionally, a small filling is placed in the end of the root canal to seal it and prevent future infections.
Once the root tip is removed and the area is thoroughly cleaned, the gum tissue is repositioned and sutured back in place. The entire procedure typically takes about 30 to 90 minutes, depending on the complexity and location of the tooth. Post-operative care is crucial for a successful recovery. Patients are advised to follow specific instructions, such as avoiding strenuous activities, maintaining oral hygiene, and taking prescribed medications to manage pain and prevent infection.
Regular follow-up visits are essential to monitor healing and ensure that the infection has been completely resolved. The apicoectomy success rate is generally high when performed by skilled professionals and followed by proper post-operative care. With advancements in dental technology and techniques, the prognosis for patients undergoing an apicoectomy has significantly improved, contributing to its effectiveness as a reliable treatment option for persistent dental infections.
Factors Influencing Apicoectomy Success Rate
Several factors can significantly influence the Apicoectomy Success Rate, making it essential to understand each one’s potential impact. First and foremost, the patient’s overall health plays a crucial role. Patients with compromised immune systems, uncontrolled diabetes, or other chronic health conditions may experience slower healing times and increased risk of complications, thereby affecting the apicoectomy success rate.
The skill and experience of the dental surgeon performing the procedure is another critical factor. A highly skilled and experienced endodontist is more likely to achieve a successful outcome due to their proficiency in handling intricate dental procedures. They are better equipped to navigate the complexities of the root structure, minimizing the chances of procedural errors. Therefore, the choice of a qualified dental professional can substantially influence the apicoectomy success rate.
The complexity of the root structure is also a significant determinant. Roots with unusual shapes, multiple canals, or those that are deeply embedded in the jawbone can present challenges during the procedure. The more complicated the root anatomy, the higher the potential for difficulties, which could impact the Apicoectomy Success Rate. Advanced imaging techniques and meticulous pre-surgical planning can help mitigate some of these challenges, but they cannot entirely eliminate the risks associated with complex root structures.
Finally, the presence of infections or complications can drastically affect outcomes. Persistent infections or severe inflammation at the surgical site can hinder the healing process and reduce the likelihood of a successful apicoectomy. Comprehensive preoperative assessments and effective postoperative care are essential to manage any infections or complications, thereby enhancing the chances of a favorable result.
Understanding these factors provides valuable insights into the variables that can influence the apicoectomy success rate, enabling both patients and dental professionals to make more informed decisions regarding the procedure.
Success Rate Statistics
Apicoectomy, a surgical procedure aimed at removing the tip of a tooth’s root along with any surrounding infected tissue, has demonstrated notable success rates over the years. According to recent studies, the average success rate for apicoectomy procedures ranges between 85% to 95%. This high success rate is indicative of the procedure’s efficacy in treating persistent infections that do not respond to conventional root canal therapy.
Historical data corroborates these findings, with older studies reporting similar success rates. A landmark study conducted in the 1990s revealed an average success rate of 90%, which aligns closely with contemporary data. These consistent results underscore the reliability and effectiveness of apicoectomy as a treatment option.
Comparisons with other dental procedures further highlight the robustness of apicoectomy outcomes. For instance, traditional root canal therapy boasts success rates of approximately 70% to 90%. While both procedures are effective, apicoectomy provides an additional solution for cases where root canal therapy alone may not suffice, particularly when addressing issues related to the root tip and surrounding tissues.
Several factors can influence the success rates of apicoectomy. Patient demographics, such as age and overall health, play a significant role. Younger patients with no underlying health conditions tend to exhibit higher success rates. Conversely, older patients or those with compromised immune systems may experience slightly lower success rates. Additionally, the skill and experience of the dental practitioner performing the procedure can significantly impact outcomes. Experienced endodontists and oral surgeons typically report higher success rates due to their advanced expertise and refined techniques.
Overall, the success rate of apicoectomy remains impressively high, making it a viable and reliable option for patients seeking resolution of persistent dental infections. The consistency of these success rates across various studies and demographics further solidifies its standing in contemporary dental practice.
What is the failure rate of apicoectomy?
While the apicoectomy success rate is notably high, it is essential to understand that not all procedures yield favorable outcomes. Various factors contribute to the failure of an apicoectomy, with incomplete removal of infected tissue being a primary concern. If remnants of the infection persist, the root canal system may remain compromised, leading to continued or recurrent symptoms. Additionally, improper sealing of the root tip can prevent proper healing and facilitate re-infection.
Patient-specific factors also play a critical role in the ultimate success of an apicoectomy. Conditions such as diabetes, smoking, and immune system disorders can impede the body’s natural healing processes, increasing the likelihood of failure. Furthermore, anatomical complexities, including curved or obstructed root canals, can present challenges that complicate the procedure.
Statistically, the failure rate of apicoectomy ranges between 10% to 20%, depending on various studies and patient demographics. This rate is relatively comparable to other endodontic treatments, such as non-surgical root canal therapy, which also exhibits a similar range of success and failure. However, it is crucial to note that these rates are influenced by several variables, including the skill and experience of the endodontist, the specific techniques employed, and the overall health of the patient.
Minimizing the risk of apicoectomy failure hinges on a multi-faceted approach. Accurate diagnosis through advanced imaging techniques and thorough evaluation of the patient’s medical history are imperative. Skilled surgical technique, honed through extensive training and experience, significantly enhances the likelihood of success. Moreover, meticulous post-operative care, including adherence to prescribed medications and follow-up appointments, ensures prompt identification and management of any complications.
By addressing these critical factors, the success rate of apicoectomy can be optimized, providing patients with a reliable solution for persistent endodontic issues.
What to Expect if an Apicoectomy Fails
While the apicoectomy success rate is generally high, there are instances where the procedure may not yield the desired results. When an apicoectomy fails, patients might continue to experience symptoms such as persistent pain, swelling, or signs of infection. It is essential to understand the subsequent steps and available treatment options to address these issues effectively.
In cases of failure, the initial recommendation often involves a thorough evaluation by your dental specialist. Retreatment of the affected area might be necessary, which could involve another apicoectomy or a different endodontic procedure to target the source of the problem. In some circumstances, more extensive surgical intervention may be required to ensure the complete removal of infected tissue and the successful sealing of the root tip.
In situations where retreatment or additional surgery does not resolve the issue, tooth extraction might be considered as a last resort. Although this outcome can be concerning for patients, advancements in dental technology offer several restorative options, such as dental implants or bridges, to replace the extracted tooth and restore functionality and aesthetics.
One of the primary concerns post-procedure is the likelihood of infection recurrence. While this risk exists, it can be mitigated through diligent oral hygiene practices and regular dental check-ups. The potential for gum tissue regeneration is another important consideration; proper care and possibly additional treatments, such as periodontal therapy, can promote healing and tissue regeneration.
The long-term survival rate of teeth treated with an apicoectomy largely depends on the success of the procedure and subsequent care. Maintaining excellent oral hygiene, including regular brushing, flossing, and professional cleanings, is crucial in supporting the longevity of the treated tooth and preventing future complications.
By adhering to these guidelines and closely monitoring your oral health, you can significantly enhance the healing process and reduce the likelihood of further issues. Consulting with your dental professional for personalized advice and follow-up care is essential for achieving optimal outcomes after an apicoectomy.
Patient Experiences and Testimonials
Patient experiences with apicoectomy procedures can provide valuable insights into the effectiveness and overall satisfaction associated with this dental surgery. A range of testimonials reveals that the apicoectomy success rate is generally high, but individual experiences vary based on factors such as pain management, recovery times, and the skill of the dental professional.
Many patients report positive outcomes, highlighting minimal pain during the procedure and a swift recovery period. One patient shared, “I was initially apprehensive about the surgery, but my dentist explained everything thoroughly. The procedure was surprisingly painless, and I was back to my normal routine within a few days.” Such testimonials underscore the importance of clear communication and skilled execution by dental professionals in achieving a high apicoectomy success rate.
However, not all experiences are uniformly positive. Some patients mention experiencing more discomfort and longer recovery times than anticipated. For instance, another patient noted, “The procedure itself was fine, but I experienced significant swelling and discomfort for about a week post-surgery. It took a bit longer to heal than I expected.” These varied experiences highlight the need for patients to have realistic expectations and to follow post-operative care instructions closely.
Common themes in patient feedback include the initial anxiety about the procedure, the effectiveness of pain management strategies, and the overall satisfaction with the surgical outcome. Most patients who successfully undergo an apicoectomy report substantial relief from their previous dental issues, contributing to the overall high apicoectomy success rate. A recurring sentiment among satisfied patients is the appreciation for their dentist’s expertise and the quality of care received.
In summary, patient testimonials provide a nuanced view of apicoectomy outcomes. While the majority reflect a high success rate and positive experiences, acknowledging the variation in individual responses is crucial for setting appropriate expectations and ensuring comprehensive patient care.
Complications and Risks
An apicoectomy, like any surgical procedure, carries certain risks and potential complications. Understanding these risks is crucial for patients considering this treatment. One of the most common complications is infection. Despite sterile techniques, bacteria can occasionally infiltrate the surgical site, leading to infection. Symptoms may include swelling, redness, and discharge. Prompt medical attention and antibiotics can effectively manage this issue.
1. Nerve damage
Nerve damage is another potential complication, albeit less common. The proximity of nerves, especially in the lower jaw, means there is a slight risk of nerve injury during the procedure. This can result in numbness, tingling, or even loss of sensation in the affected area. In most cases, these symptoms are temporary, but permanent nerve damage, although rare, is a possibility.
2. Persistent pain
Persistent pain following an apicoectomy is also a concern for some patients. While most individuals experience relief from their symptoms post-surgery, a minority may continue to suffer from discomfort. This could be due to incomplete removal of the infected tissue or other underlying conditions that need further treatment. Regular follow-ups with the dental surgeon can help in monitoring and addressing any ongoing issues.
3. Sinus perforation
In rare cases, other complications such as sinus perforation (in the upper jaw) or jawbone fracture may occur. These are uncommon but highlight the importance of selecting a skilled and experienced oral surgeon for the procedure.
Mitigating these risks involves careful pre-operative planning and adherence to post-operative care instructions. Patients are advised to follow their dentist’s guidelines meticulously, which typically include maintaining oral hygiene, taking prescribed medications, and avoiding certain activities that may strain the surgical site. Regular check-ups help in early detection and management of any complications, thereby improving the overall apicoectomy success rate.
Post-Operative Care and Recovery
Effective post-operative care is essential for ensuring the success of an apicoectomy. Patients are advised to adhere to specific guidelines to facilitate optimal healing and reduce the risk of complications. Immediately following the procedure, it is crucial to manage diet and oral hygiene carefully. Soft foods are recommended for the first few days to minimize strain on the surgical site. Examples include yogurt, mashed potatoes, and smoothies. Gradually, patients can reintroduce more solid foods as comfort allows.
Oral hygiene plays a critical role in preventing infection and promoting recovery. Patients should gently rinse their mouths with a warm saltwater solution several times a day, especially after meals. Brushing should be done cautiously, avoiding the surgical area to prevent irritation. Using an antiseptic mouthwash as recommended by the dental professional can further aid in maintaining oral cleanliness.
Activity levels should be moderated during the initial recovery period. Strenuous physical activities and heavy lifting should be avoided for at least a week post-surgery. Rest is vital, and patients should aim to keep their head elevated while sleeping to reduce swelling and discomfort. Applying ice packs intermittently during the first 24-48 hours can also help manage swelling.
Follow-up visits are an integral part of the post-operative care regimen. These appointments allow the dental professional to monitor the healing process, address any concerns, and remove sutures if necessary. It is recommended to schedule the first follow-up visit within a week of the procedure, with subsequent visits as advised by the healthcare provider.
The typical recovery timeline for an apicoectomy spans over a few weeks, with most patients experiencing significant improvement within the first two weeks. However, it is essential to remain vigilant for signs of complications. Symptoms such as persistent pain, excessive swelling, fever, or discharge from the surgical site should prompt immediate consultation with a dental professional. Addressing these issues promptly is crucial to maintaining a high apicoectomy success rate and ensuring a smooth recovery process.
Future Outlook and Advancements
The field of apicoectomy is continually evolving, with ongoing research and emerging technologies set to enhance the procedure’s effectiveness and improve patient outcomes. One notable advancement is the integration of advanced imaging techniques, such as Cone Beam Computed Tomography (CBCT). These imaging technologies provide a more precise and detailed view of the root structure and surrounding tissues, enabling more accurate diagnosis and surgical planning. As a result, the apicoectomy success rate is expected to improve, as surgeons can address the underlying issues with greater precision.
Another significant development is the advent of bioactive materials and regenerative techniques. The use of materials like Mineral Trioxide Aggregate (MTA) has shown promise in promoting the healing of periapical tissues and preventing future infections. These materials not only enhance the structural integrity of the root but also support the regeneration of bone and soft tissue, contributing to a higher success rate of apicoectomies.
Laser technology is also making headway in endodontic surgeries, including apicoectomy. Lasers offer several advantages, such as reduced bleeding, minimized postoperative pain, and enhanced sterilization of the surgical site. These benefits can lead to a smoother recovery process and lower the risk of complications, thereby positively impacting the overall apicoectomy success rate.
Ongoing research into minimally invasive surgical techniques is another area of focus. Advances in microsurgical instruments and techniques allow for smaller incisions and more precise removal of infected tissue, reducing trauma to the surrounding structures. This minimally invasive approach not only shortens recovery time but also decreases the likelihood of postoperative complications, further improving the success rates of apicoectomies.
As these technologies and techniques continue to develop, the future of apicoectomy procedures looks promising. With enhanced diagnostic tools, innovative materials, and refined surgical methods, the success rate of apicoectomies is poised to increase, offering patients better outcomes and a higher quality of dental care.
FAQs
-
What is the disadvantage of apicoectomy?
the most common complications is post-surgical pain and swelling, Infection and Less common but more serious complications include nerve damage. Another significant concern is the potential for persistent or recurring infections.
-
What is the failure rate of apicoectomy?
Statistically, the failure rate of apicoectomy ranges between 10% to 20%, depending on various studies and patient demographics.
-
What happens when an apicoectomy fails?
In situations where retreatment or additional surgery does not resolve the issue, tooth extraction might be considered as a last resort. Although this outcome can be concerning for patients, advancements in dental technology offer several restorative options, such as dental implants or bridges, to replace the extracted tooth and restore functionality and aesthetics.
-
Can infection come back after apicoectomy?
yes, While apicoectomy aims to remove the source of infection and promote healing, there is no guarantee that the infection will not return. In some cases, the tooth may still need to be extracted if the infection persists despite the procedure.
-
Do gums grow back after apicoectomy?
Yes, the good news is that gums do tend to heal well after the procedure. Following an apicoectomy, the gums and surrounding tissue typically regenerate and heal naturally over time.