Table of Contents
Introduction
The temporomandibular joint, commonly referred to as the TMJ, plays a crucial role in our daily lives, facilitating essential activities such as chewing, speaking, and yawning. This unique joint connects the jawbone, or mandible, to the temporal bones of the skull, located just in front of each ear. The TMJ’s complex structure allows it to function as both a hinge and a sliding joint, providing the flexibility and range of motion necessary for various jaw movements.
Anatomically, the TMJ consists of several key components, including the mandibular condyle, the articular disc, and the surrounding ligaments and muscles. The mandibular condyle is the rounded end of the jawbone that fits into the concave part of the temporal bone, known as the mandibular fossa. Positioned between these two bony surfaces is the articular disc, a fibrocartilaginous structure that acts as a cushion, absorbing shock and reducing friction during jaw movements.
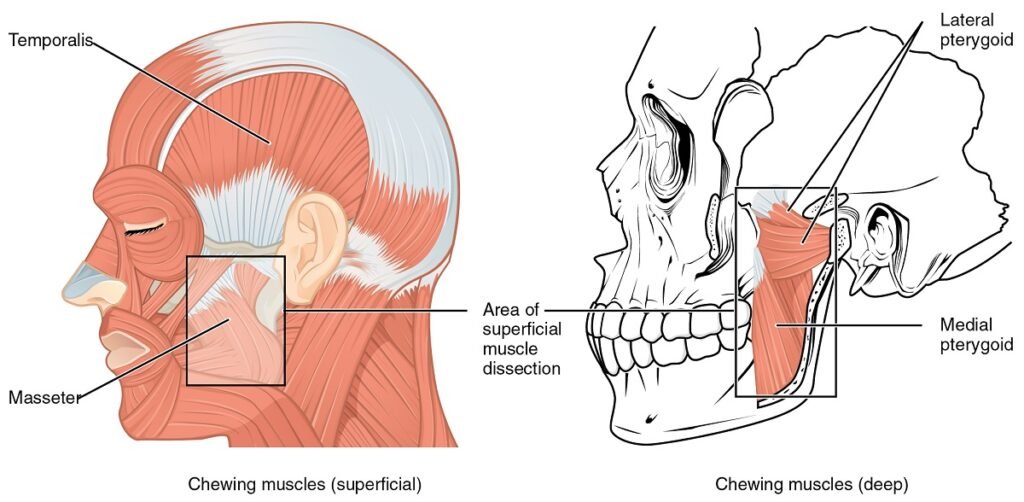
Ligaments and muscles play a vital role in stabilizing and controlling the movements of the TMJ. The lateral ligament, for instance, helps to prevent excessive forward, backward, and lateral movements of the jaw. Meanwhile, the muscles of mastication, such as the masseter and temporalis, coordinate to produce the powerful biting and chewing actions essential for processing food.
The health of the TMJ is paramount to overall oral well-being. Dysfunction of this joint can lead to a range of problems, collectively known as temporomandibular disorders (TMD). Symptoms of TMD can include pain, clicking or popping sounds, and limited jaw movement, all of which can significantly impact one’s quality of life. Understanding the anatomy and function of the TMJ is the first step in recognizing the importance of maintaining its health and addressing any issues that may arise.
Common Symptoms of TMJ Disorders
Temporomandibular joint (TMJ) disorders encompass a range of symptoms that can significantly impact daily life. One of the most prevalent indicators of TMJ disorders is jaw pain, which may manifest as a consistent, dull ache or sharp, intermittent discomfort. This pain often intensifies during activities that involve jaw movement, such as chewing, speaking, or yawning.
Another common symptom is difficulty in opening and closing the mouth. Individuals with TMJ disorders might experience a limited range of motion or feel their jaw lock in a certain position. This restriction can be particularly distressing, making routine activities like eating and speaking challenging.

Clicking or popping sounds in the jaw are also frequently reported. These noises, which occur when the jaw moves, can be accompanied by pain but are sometimes painless. They indicate an irregularity in the joint’s movement, often stemming from displaced cartilage or joint misalignment.
Muscular discomfort is another hallmark of TMJ disorders. The muscles around the jaw, face, and even the neck can become sore and tender. This muscular pain can extend beyond the immediate area of the jaw, leading to headaches and even neck pain.
Moreover, TMJ symptoms are not confined to the jaw area. Many individuals report ear-related issues, such as earaches, a feeling of fullness in the ear, or tinnitus (ringing in the ears). These symptoms occur because the temporomandibular joint is located close to the ear, and inflammation or dysfunction in the joint can affect the surrounding structures.
In some cases, TMJ disorders can lead to discomfort in the neck and shoulders, further complicating the clinical picture. This extension of symptoms highlights the interconnected nature of the musculoskeletal system and underscores the importance of a comprehensive approach to diagnosis and treatment.
TMJ and Headaches
Temporomandibular joint (TMJ) disorders are often linked with chronic headaches, a relationship that is increasingly recognized in medical literature. The TMJ, being a complex joint that connects the jaw to the skull, is instrumental in various functions like chewing and speaking. When this joint becomes dysfunctional, it can lead to a cascade of symptoms, including debilitating headaches.
The connection between TMJ disorders and headaches primarily stems from the intricate network of muscles and nerves in and around the jaw. Tension in the jaw muscles, often a result of TMJ disorders, can radiate pain to other areas of the head. This tension can manifest as tension-type headaches, characterized by a constant, dull pain that affects both sides of the head. The pain is often described as a tight band around the forehead or back of the head, and can be exacerbated by jaw movements.
Moreover, TMJ disorders can also trigger migraines, which are more severe and often accompanied by symptoms such as nausea, light sensitivity, and throbbing pain. The exact mechanism is not entirely understood, but it is believed that the inflammation and irritation in the TMJ area can affect the trigeminal nerve, which plays a crucial role in migraine pathogenesis. The trigeminal nerve is responsible for transmitting sensory information from the face to the brain, and its involvement in TMJ disorders can amplify headache symptoms.
In addition, bruxism, or teeth grinding, which is commonly associated with TMJ disorders, can further intensify headache symptoms. The repetitive clenching and grinding can put additional strain on the TMJ and surrounding muscles, leading to increased muscle tension and subsequent headaches.

Understanding the relationship between TMJ disorders and headaches is essential for effective treatment. Addressing the underlying TMJ issues can significantly alleviate headache symptoms, improving the quality of life for those affected. Therapies may include oral appliances, physical therapy, and stress management techniques to reduce muscle tension and prevent headache recurrence.
Understanding TMJ Pain
Temporomandibular joint (TMJ) disorders can manifest through various types of pain, significantly affecting an individual’s daily life. TMJ pain can be categorized into two primary types: acute and chronic.
- Acute TMJ pain is typically sudden and sharp, often resulting from trauma or a specific injury to the jaw. This type of pain can be intense but usually subsides with appropriate treatment and rest.
- On the other hand, chronic TMJ pain persists over an extended period, often becoming a constant or recurring issue. This type of pain might be dull or throbbing and can be exacerbated by activities such as chewing, speaking, or even yawning. The chronic nature of this pain can severely impact an individual’s quality of life, leading to difficulties in performing everyday tasks and contributing to emotional stress and fatigue.
TMJ pain varies not only in type but also in intensity and duration. Some individuals may experience mild discomfort that comes and goes, while others may endure severe pain that significantly disrupts their routine. The intensity of TMJ pain can fluctuate, sometimes peaking during activities that strain the jaw muscles and joints. Duration can also vary, with some episodes lasting only a few minutes, while others may persist for hours or even days.
The impact of TMJ pain on an individual’s quality of life should not be underestimated. Persistent pain can lead to reduced productivity, difficulty concentrating, and avoidance of social interactions. Additionally, the emotional toll of ongoing discomfort can contribute to anxiety and depression. Effective management of TMJ pain is crucial, not only to alleviate physical symptoms but also to enhance overall well-being and mental health.
TMJ Surgery: When and Why
Temporomandibular joint disorders, commonly referred to as TMJ, can sometimes necessitate surgical intervention, especially when conservative treatments fail to provide relief. Surgery is generally considered a last resort for TMJ disorders and is recommended only after careful evaluation by a specialist. This decision is usually based on the severity of the symptoms, the underlying cause of the disorder, and the patient’s overall health.
There are several types of surgical procedures available for TMJ disorders. Arthrocentesis is a minimally invasive procedure that involves flushing out the joint with a sterile solution to remove debris and inflammatory byproducts. It is often used for patients with limited jaw movement and pain. Arthroscopy, another minimally invasive option, involves inserting a small camera and instruments into the joint to diagnose and treat issues such as adhesions or damaged tissue.

For more severe cases, open-joint surgery might be necessary. This procedure allows direct access to the temporomandibular joint, enabling the surgeon to repair or replace the joint structures. While open-joint surgery can be highly effective, it comes with increased risks, including infection, nerve damage, and a longer recovery period. Total joint replacement is another surgical option, primarily reserved for patients with severe joint damage due to arthritis or trauma. This procedure involves replacing the damaged joint with a prosthetic one, which can significantly improve function and reduce pain.
The potential benefits of TMJ surgery include pain relief, improved jaw function, and enhanced quality of life. However, it’s essential to weigh these benefits against the possible risks. Patients should have a thorough discussion with their healthcare provider to understand the potential outcomes and recovery expectations. Recovery from TMJ surgery can vary, but it typically involves a combination of physical therapy, pain management, and dietary modifications to ensure optimal healing and functionality.
In summary, TMJ surgery is a critical option for those suffering from severe TMJ disorders unresponsive to conservative treatments. Understanding the various surgical options and their associated risks and benefits can help patients make informed decisions about their care.
Effective TMJ Exercises
For those experiencing the discomfort and pain associated with TMJ, incorporating regular exercises into their routine can be highly beneficial. These exercises are designed to strengthen the jaw muscles, enhance flexibility, and alleviate tension, ultimately helping to manage TMJ symptoms more effectively.
One of the fundamental exercises is the relaxation exercise, which involves placing the tongue on the roof of the mouth while allowing the teeth to come apart. This exercise helps to reduce tension in the jaw muscles and should be done several times a day for optimal results.
Another crucial exercise is the goldfish exercise. For this, place one finger on the TMJ and another finger on your chin. Drop your lower jaw halfway and then close it. You should feel a mild resistance but not pain. Repeat this exercise six times in one set and perform at least three sets daily to improve jaw mobility and reduce tightness.
The resisted opening exercise is also effective. Place your thumb under your chin and gently push down while attempting to open your mouth. This resistance helps to strengthen the muscles around the jaw. Hold the position for a few seconds before closing your mouth. Repeat this exercise ten times, ensuring that the movements are slow and controlled.
Additionally, the chin tuck exercise can aid in improving jaw alignment. Sit or stand with your back straight and pull your chin straight back, creating a “double chin” effect. Hold this position for a few seconds and then release. Performing this exercise several times a day can help in maintaining proper posture and reducing TMJ strain.
Consistency and proper technique are critical when performing these exercises. It is advisable to start slowly and gradually increase the intensity to avoid exacerbating symptoms. Consulting with a healthcare professional before beginning any new exercise regimen is always recommended to ensure safety and effectiveness.
Anatomy of the TMJ
The temporomandibular joint (TMJ) is a sophisticated structure that plays a critical role in various functions such as chewing, speaking, and swallowing. Located on each side of the head, the TMJ connects the mandible, or lower jaw, to the temporal bone of the skull. This joint is unique in that it is both a hinge joint and a sliding joint, allowing for complex movements necessary for daily activities.
The primary components of the TMJ include bones, muscles, and ligaments. The mandible and the temporal bone form the bony framework of the joint. Between these bones lies an articular disc made of fibrocartilage, which acts as a cushion to absorb shocks and facilitate smooth movements. This disc divides the joint into two compartments, each filled with synovial fluid that lubricates the joint, reducing friction and wear.
Muscles surrounding the TMJ are vital for its function. The major muscles involved include the masseter, temporalis, medial pterygoid, and lateral pterygoid. These muscles work in harmony to enable the jaw’s movements, such as opening, closing, and side-to-side motion. Ligaments, such as the temporomandibular ligament, sphenomandibular ligament, and stylomandibular ligament, provide stability and limit the range of motion, preventing dislocation.
Dysfunction in any part of this intricate system can lead to TMJ disorders. For instance, a misaligned articular disc can result in clicking or popping sounds and pain during jaw movements. Muscle tension or spasms can cause restricted movement and discomfort. Ligament damage or inflammation can lead to instability and chronic pain. Understanding the detailed anatomy of the TMJ is essential for diagnosing and treating TMJ disorders effectively, ensuring that each component is evaluated to identify the root cause of dysfunction.
Managing TMJ Dysfunction
Managing TMJ dysfunction requires a multifaceted approach, incorporating both lifestyle modifications and professional medical interventions. An effective strategy often begins with simple home remedies and progresses to more advanced treatments, depending on the severity of the condition.
First and foremost, lifestyle changes play a significant role in alleviating TMJ symptoms. Patients are encouraged to adopt a soft diet to minimize jaw strain, avoid chewing gum, and practice stress reduction techniques such as mindfulness and meditation. These measures can help reduce the frequency and intensity of TMJ pain.
Home remedies also serve as a first line of defense. Applying heat or cold packs to the affected area can offer temporary relief from pain and inflammation. Gentle jaw exercises, under the guidance of a healthcare professional, can improve jaw function and reduce stiffness.
When these initial steps are insufficient, medical treatments become necessary. Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to manage pain and inflammation. In some cases, muscle relaxants or low-dose antidepressants may be recommended to address chronic pain and muscle tension associated with TMJ dysfunction.
Physical therapy is another crucial component of managing TMJ. A trained physical therapist can provide specialized exercises and manual techniques to improve jaw mobility and reduce discomfort. Additionally, dental interventions, such as occlusal splints or mouthguards, can help correct bite issues and prevent teeth grinding, further alleviating TMJ symptoms.
In more severe cases, surgical options may be considered. These include arthrocentesis, arthroscopy, or open-joint surgery, each tailored to address specific TMJ dysfunctions. However, surgery is typically viewed as a last resort after conservative treatments have been exhausted.
The importance of a multidisciplinary approach cannot be overstated. Collaboration between dentists, physical therapists, and medical doctors is essential to develop a comprehensive treatment plan tailored to the individual’s needs. This team-based strategy ensures that all aspects of TMJ dysfunction are addressed, optimizing patient outcomes.
FAQs
-
How do you fix TMJ issues?
Treatment for TMJ disorders can vary based on the severity and underlying cause. Options range from conservative treatments like physical therapy, stress management, and the use of mouthguards to more invasive procedures such as injections or surgery. Consulting a healthcare provider is essential for a tailored treatment plan.
-
Can I treat TMJ myself?
While self-care practices can help manage mild TMJ symptoms, it’s important to consult a healthcare provider for an accurate diagnosis and treatment plan. Self-care options include applying ice or heat to the jaw, performing gentle jaw exercises, and avoiding hard or chewy foods. Stress-reduction techniques can also be beneficial.
-
Is TMJ a lifelong condition?
TMJ disorders are not necessarily lifelong conditions. Many people experience temporary symptoms that can be managed effectively with appropriate treatment. However, chronic cases may require ongoing management strategies to alleviate symptoms.
-
What is TMJ caused by?
TMJ disorders can be caused by various factors, including genetics, arthritis, or jaw injury. Bruxism, or the habit of grinding teeth, is another common cause. Stress can also contribute to muscle tension and exacerbate TMJ symptoms.